PERSPECTIVES: How can social media and communications technologies be better harnessed to increase uptake of HIV testing among key populations?
Published Wednesday, March 23, 2018
We asked four experts who work with people at high risk for HIV in Asia how new technologies can best link them to testing and care.
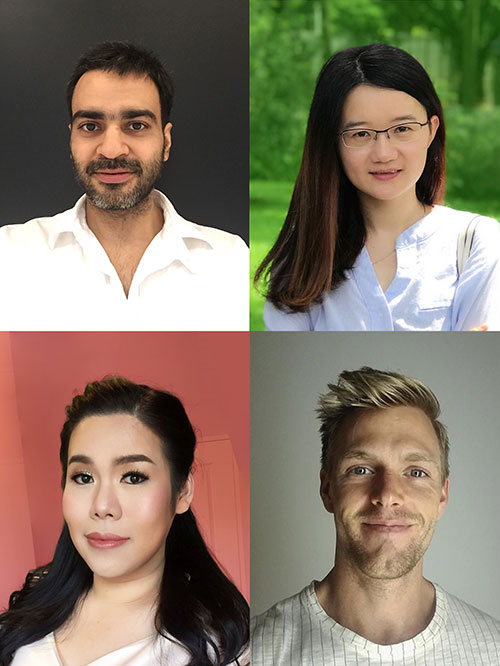
(Clockwise, from top left) Tarandeep Anand, Bolin Cao, Benjamin Eveslage, Rena Janamnuaysook.
Tarandeep Anand is the founder and director of Adam’s Love (adamslove.org), and has been a TREAT Asia research partner since 2011.
How “emerging technologies can be harnessed to increase HIV testing” is what I had inquired back in 2010, and led to the establishment of Adam’s Love and TemanTeman.org, major HIV services scale-up innovations for MSM and Transgender women (TG), now serving millions of online key populations globally and offering sexual risk, behavioral counseling and linkage support to over 25,000 MSM, TG and youth annually.
As we get swept away by the “Amazon effect,” witness blurring lines between online and offline worlds, a sense of urgency to transform HIV service delivery is apparent. I will try to reflect on where we are and how we can benefit from the technology tailwinds to help implementers scale-up services.
1. Online-to-Offline (O2O) models. My instant response is to use O2O models that enable seamless transition, dramatically reduce the linkage time and demonstrate high linkage success. Digital bookings and QR codes used help ensure key populations confidentiality.
2. Chatbots vs. human interaction. A person recently exposed to HIV is often in desperate need for human support/counseling as opposed to automated responses. Online channels operate 24x7 and have no time or logistic barriers. This is where most initiatives run out of gas, get cumbersome for implementers and result in lost interest among users seeking instant gratification, so identifying passionate professionals is key.
3. Performance incentives. In recent HIV self-testing study supported by amfAR, we found that digital literacy and ICT skills are intrinsically high among Thai counselors/communities. Incentivizing online staffs who deliver indispensable services based on targets achieved, could have a major impact on the epidemic. Paying social media giants to promote testing advertisements might help researcher enhance recruitment on a one-time basis, but this is not a sustainable path.
4. Emphasize digital culture. The implementers of most technology-based interventions are public health experts with limited background in technology, marketing or customer service. An innovative workforce with appropriate background would bring fresh synergies.
5. Understand what you fund. To create “blue oceans,” funders should employ experts well-versed with important parameters for adequate assessments of tech programs, sustain what is working, and harness published data as value for setting standards for funding.

Adam’s Love participant recruited online receives offline HIV services and O2O campaign incentives. (Photo: Tarandeep Anand)
Bolin Cao is an Assistant Professor at the School of Media and Communication, Shenzhen University in Shenzhen, China. She was previously a postdoctoral fellow at the University of North Carolina Project–China, leading a social media team to spur HIV testing among Chinese MSM.
Social media can play multiple roles to drive HIV testing among key populations. As information providers, social media not only allows key populations to access much HIV-related information, but also to actively seek and publish content related to HIV testing. As service providers, social media can serve as platforms to link key populations to healthcare services, such as offering HIV self-testing kits online and providing pre-test consultation. As crowdsourcing platforms, social media can help crowdsource ideas from key populations to design more effective interventions. As communities, social media enables key populations to get connected, and the peer-led communities can facilitate men to get HIV tested and provide social support. Overall, social media brings many opportunities for healthcare providers to reach key populations, especially MSM.
For more information, see: http://www.jmir.org/2017/11/e394.
Benjamin Eveslage is a Technical Officer with the LINKAGES Project, FHI 360, working with their Asia-Pacific Regional Office to support technology-driven approaches to improve service uptake.
As of 2018, there are an estimated 4 billion internet users worldwide, with the Asia region particularly well-connected.1 Key populations (KPs) look to these platforms to find friends and sexual partners quickly, and with fewer perceived risks. Going online will accelerate the impact of KP HIV programs in Asia, and will keep these programs relevant in a dramatically changing digital landscape. The USAID- and PEPFAR-funded LINKAGES project in several Asian countries uses a four-part online approach to improve HIV testing uptake and service retention:
1. identify unreached online KPs,
2. target communications to reach and link these online KP to offline HIV services,
3. support KPs’ continuous engagement in HIV services, and
4. use data to assess and improve models, targeting and performance.
Using new mapping approaches, the LINKAGES program identified an average of 7,000 online MSM on the popular gay dating app Grindr in metro Mumbai, and found six locations of dense Grindr usage to inform peer outreach on mobile dating apps. In Indonesia, Civil Society Organizations mapped over 100 social media influencers with a large following of MSM and other KPs, and developed plans to engage influencers in a broad testing campaign. Online influencers in Thailand served as “super recruiters” referring hundreds of additional clients to HIV testing at minimal cost to the program. And in both Thailand and Nepal, LINKAGES leveraged social media marketing data to target ads towards KPs, link them to a risk assessment tool, and find nearby HIV services or book appointments. In Thailand, this resulted in increased case-finding among clients reached by targeted ads on social media platforms compared to clients recruited through venue-based outreach during the same period.
HIV programs in Asia are learning how going online can better meet KPs in the increasing virtual places where they can be reached and offer HIV information and services that address the wide range of KP service needs and preferences. HIV programs need to continue innovating by leveraging online and social media platforms to accelerate impact and more effectively reach an AIDS free generation.
Co-written with Matt Avery, Associate Regional Technical Director–Asia-Pacific Regional Office, FHI 360.
1Hootsuite (2018, January). We Are Social: Digital in 2018 in Southeast Asia part 2. See: https://templatelab.com/global-digital-report/#page=471

Crowdsourced images to facilitate HIV testing (Image: Bolin Cao)
Rena Janamnuaysook is a program coordinator at the Thai Red Cross AIDS Research Centre, working with the USAID-funded LINKAGES Thailand Project. She also supports the Tangerine Community Health Center, Southeast Asia's first transgender-specific sexual health clinic.
Social media and communications technologies play significant roles in daily life. They provide a platform for key populations (KPs) to be themselves by disclosing their sexual orientation, gender identity and gender expression. Whereas in the real world, including in the public health arena, they are prevented from accessing such a safe space due to stigma and discrimination based on who they are and what they do. In ending AIDS, HIV interventions need to be adapted based on the specific health needs of KPs and their risk behaviors, and therefore, meaningful participation of KPs is essential.
Social media led by KPs works effectively in increasing HIV service uptake. A study supported by amfAR showed that the HIV-positive yield and the first-time HIV testers among men who have sex with men (MSM) reached by online supervised peer-mediated HIV self-testing was higher than those who presented for HIV testing at community health centers. To avoid tokenistic use of KPs, engaging them in the design and implementation is necessary. This will allow delivery of well-tailored, high-impact, and innovative programs, that respond to their unmet health needs. For example, Tangerine Community Health Center at the Thai Red Cross AIDS Research Centre worked with transgender celebrities as social media influencers to promote a comprehensive health service package among Thai transgender women (TGW) on Facebook Live. Because, gender-affirmative hormone treatment was their main interest, we integrated HIV and other sexual health services in the sessions. As a result, the HIV testing uptake among TGW significantly increased three times in the last quarter, the HIV-positive yield was even higher, and almost 100% were linked to care after their diagnosis.
Real-time services must be made available and include online counseling and HIV self-testing, where healthcare providers can supervise and facilitate the process through interactive platforms including web chats and video calls. Moreover, online service systems must be linked with door-to-door delivery services, ranging from pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) as well as harm reduction. There should be reliable referral systems in place for HIV confirmatory testing, STI screening, antiretroviral treatment and other psychosocial support. Only then can we end AIDS among key populations.