Posted by Lucile Scott, November 6, 2015

A nurse at the Myanmar Ministry of Health’s AIDS/STD Prevention and Control Programme
In March 2011, Myanmar’s 50-year old military junta was officially dissolved, nominally ending the world’s longest-running military dictatorship and opening the nation’s previously impermeable borders to international economic and political actors, from Coca Cola to the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). This Sunday, the country will hold elections widely viewed by the citizens of Myanmar—and the world—as a critical test of whether recent reforms genuinely signaled the start of a transition to democracy or just the continuation of authoritarianism under a new guise.
Regardless of whether this weekend’s election is viewed as free and fair, things are definitely changing in the country of 51 million, including its national response to HIV. And an amfAR-funded implementation science project to improve HIV testing and treatment access among gay men, other men who have sex with men (MSM), and transgender individuals (collectively, GMT) is on the front line of that evolving strategy.

The Alliance’s Kaung Htet Thu
“Myanmar was inaccessible to global research prior to 2011, so this study will shed light on what obstacles there are to linkages to HIV treatment and care among GMT,” says Sandra Hsu Hnin Mon, who is originally from Myanmar and is a student investigator at the Johns Hopkins Bloomberg School of Public Health, one of several institutions collaborating on the project.
In a 2000 World Health Organization (WHO) ranking of world health systems, Myanmar came in second to last, ahead of only Sierra Leone. But in 2013, the government began increasing health spending and reforming its dilapidated healthcare system. It did away with a strict quota system that greatly restricted the number of individuals who could access antiretroviral therapy (ART), changing the threshold for ART eligibility from a CD4 count of 150 (below the 200 count used to establish an AIDS diagnosis) to 350, and then, this year, to 500, in keeping with WHO guidelines.

The Myanmar Youth Star Network’s Aye Nyein Myitta
This, combined with an influx of funding from PEPFAR, the Global Fund to Fight AIDS, Tuberculosis and Malaria, and other international donors, means that ART is now more widely available; however, only 40% of people living with HIV in Myanmar are currently on treatment—a dangerously low rate of access caused in part by extremely low HIV awareness and testing rates. According to the country’s 2015 Global AIDS Response Progress Report, only 48% of MSM have ever been tested for HIV.
“As the government changed, they increased the budget for health and HIV and allowed civil society to participate in the national response,” says Dr. Soe Naing, executive director of International HIV/AIDS Alliance Myanmar. “Now patients can get treatment, but the problem is we have to find out who the patients who need treatment are.”
Same-sex sexual activity is illegal in Myanmar, and while prosecutions under the law, known as Section 377, are rare and many GMT individuals in urban areas live openly, stigma and discrimination remain rampant, preventing many community members from accessing HIV testing and care at government clinics. In the amfAR-funded study, the Alliance and John Hopkins are working in collaboration with the Myanmar Ministry of Health, the University of Public Health of Myanmar, and two community-based organizations, the Myanmar MSM Network and the Myanmar Youth Star Network, to reach marginalized and “hidden” populations by using new and innovative HIV testing and treatment technologies.

A nurse with a patient at the AIDS/STD Prevention and Control Programme
These include home-based HIV self-testing, point-of-care CD4 testing—which can determine a patient’s treatment eligibility in minutes, without requiring them to return to the clinic for results—and having peer navigators familiar with the health system help those who test positive access GMT-friendly healthcare and adhere to treatment. The researchers plan to launch the intervention and data collection phase of the study, which will take place in Yangon, later this month.
“These innovations are very new to Myanmar,” says Kaung Htet Thu, research coordinator at the Alliance, which provides both testing and treatment. “Previously, we lost patients to follow-up while waiting to get their CD4 test results, and self-testing with OraQuick will be a great solution [to address low testing rates] because confidentiality is key to privacy and dignity.”
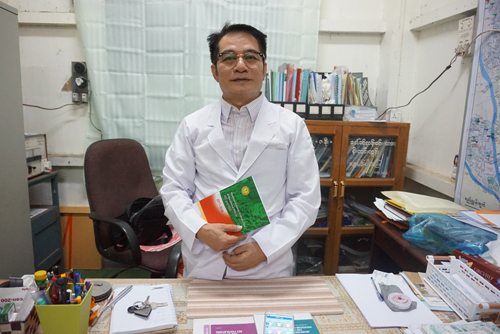
Dr. Myo Thant
After celebrating the nation’s first public same-sex commitment ceremony with his partner in 2014, Aye Nyein Myitta, project coordinator of Myanmar Youth Star Network, became a symbol of the burgeoning gay rights movement in the country. He is one of the members of the community contributing to the study’s design and implementation, ensuring it meets the diverse needs of affected individuals. “The strength of this project is that it will reach the many hidden GMT, who are educated and uneducated and from all socioeconomic statuses,” says Myitta. “It will also cause the larger community to recognize that we as a LGBT community are able to carry out these important projects.”
The study includes two arms: participants receiving the newer interventions and those receiving more traditional methods of testing and care at GMT-friendly clinics. This design will allow the team to generate definitive data regarding the innovative strategies’ effectiveness—data that can then be used to advocate scaling up effective interventions throughout Myanmar and in other resource-limited settings.

A street in downtown Yangon
“We will use this research to make recommendations to the government for it to implement in its future programs,” says Dr. Myo Thant, a regional officer of the Ministry of Health’s National AIDS Program, who will serve as a lead researcher on the project.
Despite the progress, many challenges to improving the national response to HIV remain, including the persistence of Section 377, doubts that the healthcare infrastructure can effectively absorb the influx of international HIV funding, and speculation that the government may be deliberately underreporting HIV statistics. But in Yangon, on the eve of the election, the talk is of hope and change. “Compared with the old days, things are really improving,” says Dr. Naing. “And we are still in the process of fighting.”