Breaking a “Vicious Circle”: Controlling HIV Reservoirs by Targeting Inflammation
Jeffrey Laurence, M.D.
Published Friday, April 11th, 2016
HIV persists in immune cells and in certain tissue compartments such as the brain and gut despite our best antiretroviral therapies (ART). Writing in the March issue of Current Opinion in HIV and AIDS, amfAR-funded scientists Marta Massanella, Rémi Fromentin, and Nicolas Chomont, all from the University of Montreal, focus on persistent inflammation in ART-treated individuals as a major driver of such viral persistence.
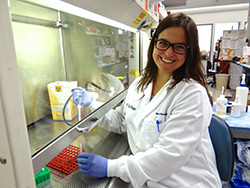 Dr. Marta Massanella Massanella and colleagues review multiple clinical and test-tube studies documenting that HIV persistence, measured by ultrasensitive lab techniques, and inflammation, assessed by “biomarkers” such as immune hormones or cytokines, are interdependent processes in HIV infection. Indeed, they “fuel each other in a ‘vicious circle,’ and that circle appears difficult to interrupt,” say the authors. Therapeutic strategies that can intervene in this positive feedback loop between inflammation and viral persistence are needed. “Most likely,” the researchers argue, “breaking the vicious circle will require targeting both phenomena concomitantly.”
Dr. Marta Massanella Massanella and colleagues review multiple clinical and test-tube studies documenting that HIV persistence, measured by ultrasensitive lab techniques, and inflammation, assessed by “biomarkers” such as immune hormones or cytokines, are interdependent processes in HIV infection. Indeed, they “fuel each other in a ‘vicious circle,’ and that circle appears difficult to interrupt,” say the authors. Therapeutic strategies that can intervene in this positive feedback loop between inflammation and viral persistence are needed. “Most likely,” the researchers argue, “breaking the vicious circle will require targeting both phenomena concomitantly.”
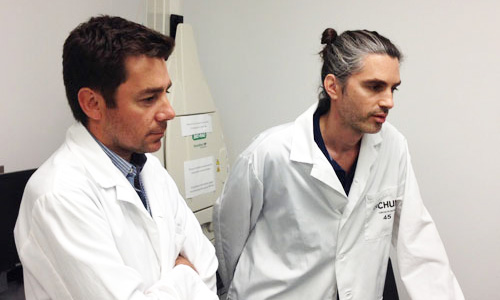 Drs. Nicolas Chomont (left) and Rémi FromentinAnd what might those interventions look like? First, the authors note that anatomical sites with relatively low ART penetration compared to blood would favor residual levels of HIV replication in those tissues. Different ART intensification strategies—that is, using more drugs with expanded profiles--could reduce residual viral replication. For example, antiretrovirals with good tissue penetration, such as the integrase inhibitor raltegravir, could be coupled with antiretrovirals that also have anti-inflammatory activity, such as the viral entry inhibitor maraviroc.
Drs. Nicolas Chomont (left) and Rémi FromentinAnd what might those interventions look like? First, the authors note that anatomical sites with relatively low ART penetration compared to blood would favor residual levels of HIV replication in those tissues. Different ART intensification strategies—that is, using more drugs with expanded profiles--could reduce residual viral replication. For example, antiretrovirals with good tissue penetration, such as the integrase inhibitor raltegravir, could be coupled with antiretrovirals that also have anti-inflammatory activity, such as the viral entry inhibitor maraviroc.
Focusing on relatively neglected cell types may also help. They note that CD4+ T regulatory cells, or Tregs, are a key modulator of inflammatory pathways. Higher levels of activated Tregs may be associated with higher levels of inflammation, and their activity can be regulated by clinically useful cytokines.
So while many investigators focus on virus-directed cure strategies, including “shock and kill” approaches and gene therapies, Massanella and associates urge further research on residual inflammation during ART as a critical parameter contributing to HIV persistence, and a block to a cure.
Dr. Laurence is amfAR’s senior scientific consultant.