
The human papillomavirus
Every year, more than 500,000 women develop cervical cancer and 270,000 women die from the disease. In Southeast Asia, it is the second most common cancer in women, with roughly 175,000 new diagnoses annually. Virtually all cervical cancer cases, as well as more than 90% of all anal cancers, are caused by the human papillomavirus (HPV). HIV and HPV are dual epidemics that fuel each other in a deadly vicious circle: people living with HIV are at higher risk of contracting HPV and developing HPV-associated cancers, while infection with HPV increases susceptibility to HIV.
A new report from TREAT Asia in collaboration with amfAR’s Public Policy Office documents the slow uptake of HPV vaccination to prevent cervical cancer in the region and the impact of these delays on the epidemiology of the disease. Since 2008, three highly effective HPV vaccines have been developed and approved in more than 100 countries. These vaccines offer an opportunity to provide population-level protection against cervical cancer in a way that is not feasible through screening alone.
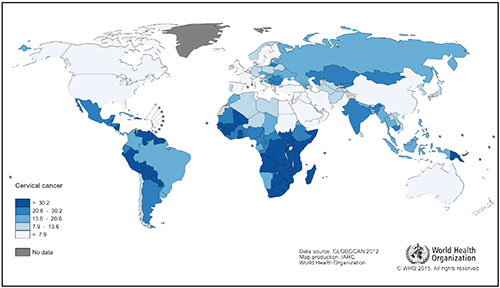
Age-standardized incidence rate of cervical cancer per 100,000 females in 20121
“Despite the proven effectiveness of HPV vaccines and the high burden of HPV-associated illnesses and mortality, many in the region who could benefit from the vaccines still do not receive them,” said Jennifer Sherwood, a policy associate at amfAR and a primary author of the new report. “Licensing agreements for the vaccines and implementation of national programs vary across countries, as does eligibility for financial support from Gavi, the Vaccine Alliance, which is the major donor enabling low-income countries to procure essential vaccines.”
The amfAR report describes lessons learned from countries that have implemented HPV vaccination programs. It recommends that all countries eligible for Gavi funding apply for it, and details steps that countries can take, such as including childhood HPV vaccination as part of comprehensive cancer prevention programs and by offering vaccinations through school-based or community delivery systems.
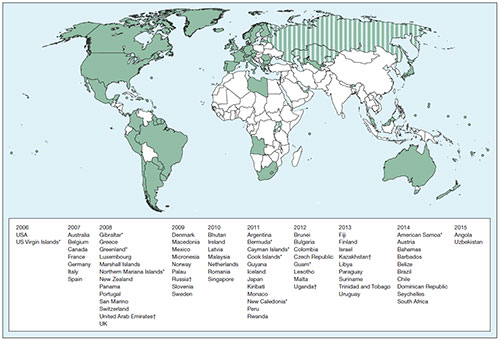
Countries with publicly funded HPV vaccination programs2
Countries with national HPV vaccination programs are in green, those with programs in only part of the country are in stripes, and those without known programs are in white.
*Special territory †Partial implementation
The Lancet Global Health, © 2016 Bruni et al.
“HPV vaccination is safe and can be cost-effective in Southeast Asia,” said Dr. Annette Sohn, director of TREAT Asia. “By developing collaborative funding arrangements and innovative delivery strategies, regional public health programs can successfully prevent cervical cancer. This is particularly important for women living with HIV.”
Read the full report, Cervical Cancer, Human Papillomavirus (HPV), and HPV Vaccines in Southeast Asia: Key Considerations for Expanding Vaccine Coverage and Improving Population Health.
A4 size
8 ½” x 11” size
1GLOBOCAN. 2012. Estimated Cervical Cancer Incidence Worldwide in 2012. International Agency for Research on Cancer, World Health Organization. Available at http://globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp
2Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, de Sanjosé S, Castellsagué X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016 Jul;4(7):e453-63. doi: 10.1016/S2214-109X(16)30099-7.